You have 2 lungs in your body. Your right lung has 3 parts. Your left lung has 2 parts. These parts are called lobes.
A wedge resection is the removal of a small, wedge-shaped part of lung tissue from a lobe of your lung.
Pre-Admission Visit
You will have an appointment at the
Pre-Admission Clinic within 2 weeks before your operation. This visit is very important to assess your health and help you prepare for your surgery and recovery. Plan for your visit to take 2 to 5 hours. On the day of your pre-admission visit, take your medications and eat as usual, unless you were given other instructions.
What should I bring to my pre-admission appointment?
- Your health card (OHIP card). If you do not have an OHIP card, please bring another form of government-issued photo ID, such as a driver's license or passport.
- Any other insurance cards. You will need the policy number of your extended health insurance, if you have any.
- Your spouse/partner, a trusted friend or family member (to offer you support and be a second set of ears).
- All the medications you take in their original containers. This includes prescription medications, over-the-counter medicines, vitamins, supplements and herbal or natural products.
- A copy of your power of attorney for personal care and/or advanced directives.
- A list of any questions that you may have about the operation and recovery.
- The name or phone number of your pharmacy, as well as any medical specialists that you have seen in the past 3 years.
- If you have had a cardiac stress test, echocardiogram and/or a pulmonary function test in the past 3 years, it would be helpful to bring a copy of the final report with you to this appointment.
What happens during my pre-admission visit?
- You will have blood tests and routine skin swabs. The swabs are taken from your nose and other areas of your body to check for germs that can cause infections.
- You may also need an
electrocardiogram (ECG) to check your heart and a chest
x-ray to check your lungs.
- You will meet many health care providers during your pre-admission visit. Please feel free to ask them any questions that you may have.
- A pre-admission nurse will review your health history and give you information to prepare you for your operation, including directions for cleaning your skin, eating before your operation, taking your medications and pain management.
- A pharmacist will review your medications.
Depending on your needs, you may also meet:
- An anesthetist who will review your health history, discuss your anesthetic plan and pain relief after your operation.
- A member of the medicine team, if you have other complex health problems.
The night before your surgery
- Do not eat or drink after midnight on the night before your operation.
- If you smoke, do not do so for 24 hours before your operation.
- Do not drink alcohol for 24 hours before your operation.
- Remove all nail polish and body piercings.
- You must have a shower with soap and water to clean your skin the night before and the morning of your surgery to reduce the chance of infection after your operation.
Stop smoking before your surgery: learn how smoking and tobacco can affect your recovery after surgery, and how
quitting can improve your health.
WHAT SHOULD I DO THE DAY OF MY SURGERY?
Arrive
2 hours before your scheduled operation time.
Surgical Admission Unit (SAU) at
Toronto General Hospital
Peter Munk Building – 2nd Floor
All hospital entrances are open by 6:00 am. However, Elizabeth St. and University Ave. are easiest to access.
You will stay in the
Post Anesthesia Care Unit (PACU) for a few hours. Once you are awake and stable, we will take you up to the
Thoracic Surgery and Respirology Inpatient Unit.
What can I expect to have on my body?
You will be attached to some or all of these machines and tubes:
| Incisions, tubes or drains | What to expect |
|---|
|
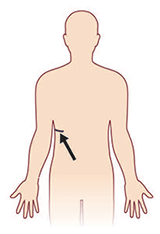
Incisions: Your surgery will be completed either by a thoracotomy or by video assisted surgery (VATS). With a thoracotomy, you will have an incision on your side: 8 to 25 centimetres (about 2½ to 10 inches) long. With VATS, you will have 3 to 5 small incisions on your side: each about 2 centimetres (about ¾ of an inch) long. You will also have 1 to 2 small incisions on your side for the chest tube(s): each will be about 2 centimetres (about ¾ of an inch) long. |
|
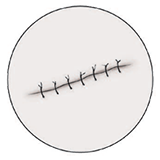
Stitches or staples: Your surgeon usually uses dissolvable stitches to close your incisions. This means they go away on their own. If your stitches or staples need to remain in after you are discharged home, your family doctor can remove them. |

|
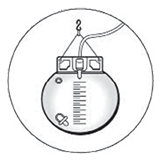
Chest tubes: You will have 1 to 2 chest tubes coming out of the side of your chest. These tubes remove air and fluid from the inside of your chest area. The tubes are attached to a machine that helps suck the air and fluid out. |
|
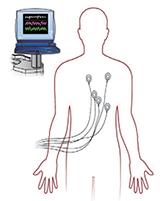
Heart monitor: You will be on a heart monitor while you are in the Step Down Unit. |
|
Urinary catheter: You will have a tube draining your bladder. |

|
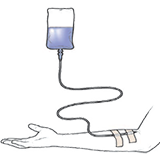
Intravenous (IV): You have an IV so we can give you fluids and medicines. It stays in until you are drinking well. |
|
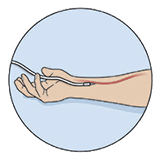
Arterial line: This tube looks like an IV, and we use it to take blood samples without having to poke you with a needle and also, to closely monitor your blood pressure. |

|
Oxygen: You may need oxygen after your operation. You get the oxygen either by facemask or through your nostrils (nasal prongs). |
HOW CAN I MANAGE MY PAIN?
We will work with you to manage your pain. We can give you pain medicine in different ways:
| Pain relief method | How it works |
|---|
|
Epidural: With an epidural, a doctor puts a small tube in your back. They usually do this right before your surgery. The tube is left in place to give you pain medicine after your surgery. It's attached to a pump, which gives you the medicines. |
|
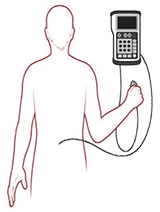
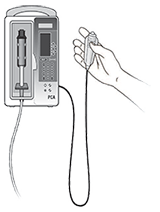
Intravenous (IV) Patient Controlled Analgesic (PCA): A PCA pump is connected to your IV that gives you pain medicine through your IV when you push the button. |
|
Intravenous (IV) medicine: You get your pain medicine through an IV. |
|
Medicine by mouth: You may get your pain medicine in tablets that you swallow. This will happen once you are drinking fluids. Let your nurse know when you have pain, so they can give you the pain medicine. |
You will continue to recover when you return home.
| Activity | How to manage at home |
|---|
| - Your appetite should return to normal within a few days. It should improve as you start to feel better and your activities increase.
- If your appetite is poor, try eating smaller meals more often.
- Add bran, high-fibre breads and cereals, berries, dried fruit or prune juice to your diet (unless your doctor or dietitian gave you different instructions).
|

| - Constipation is a common problem when taking pain medicine
- Drink plenty of fluids (at least 6 cups a day unless your doctor or dietitian gave you different instructions).
|

| - Keep your incisions clean and dry.
- You don't have to cover your incisions. If your clothes are rubbing on your incisions, you can cover them with clean gauze.
|

| - You can shower once you get home, and you should shower each day. Use a mild soap and let the water run over your incisions. Pat the incisions dry with a towel. Don’t rub.
|

| - You can gradually increase your activity when you get home. Go for a walk at least once a day if you can. Wait 2 to 3 weeks before you swim. You can golf after about 3 to 4 weeks. Wait 4 weeks before you start jogging, playing tennis or racquetball, or doing aerobics.
|

| - You should expect to be off work for at least 2 to 4 weeks. Depending on your job, you may need to be off longer. Ask your surgeon when it's safe for you to return to work.
|

| - No heavy lifting, carrying, pushing or pulling for 4 weeks.
- You can lift up to 10 pounds (about 5 kilograms).
|

| - You can start having sex whenever you feel more comfortable (have less pain and more energy). Choose positions that won't put stress on your incisions.
|
| - Don't drive until you are off all pain medicine. You must be able to fully move your arm and shoulder before you can safely steer a car. This usually takes about 2 to 3 weeks after surgery.
|
| - Please check with your surgeon about travelling. We usually recommend you not travel by air for 2 to 3 weeks after your operation.
|
Where and when
About 4 to 6 weeks after your operation you will have an appointment at your surgeon's office and the
Medical Imaging Department.
