
UHN's Delirium Prevention and Management Steering Committee consists of inter-professional team members from across the organization. (Photo: UHN)
It is estimated that up to 70 per cent of ICU patients and 30 per cent of inpatients will experience delirium in Canada this year.
Mila is one of those patients.
Delirium is a condition that causes a disturbance of consciousness. It happens quickly and can fluctuate over time. Patients experiencing hyper-active delirium may be very restless and agitated while hypo-active delirious patients may go undiagnosed as they tend to be withdrawn and quiet. Patients with delirium may experience hallucinations and perceptual disturbances.
Mila was admitted to hospital for surgery when she began experiencing delirium. Her mother was at the bedside in tears.
After speaking with Mila and her mother, her care team discovered her sister had died one year ago to the day in the very same hospital room.
Recognizing that delirium is a condition better managed by natural light, Mila's care team swiftly facilitated a move to a room with a window at the other side of the unit.
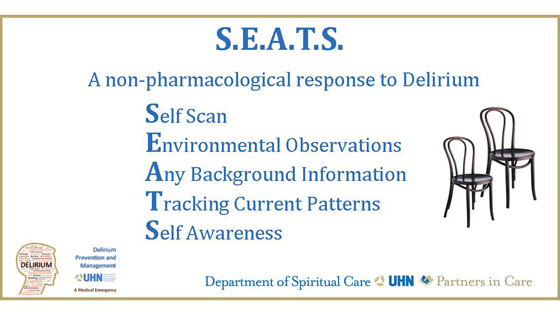
S.E.A.T.S. is a new approach to treating delirium without the use of medication.
(Photo: UHN)
Spiritual Care pilots new approach to treating delirium
By understanding Mila's personal experience and background information, her care team was able to facilitate a successful intervention using a new reflective model developed by the Department of Spiritual Care.
In September, Spiritual Care will pilot S.E.A.T.S. in the Intensive Care Unit at Toronto Western, a new model for treating delirium patients without the use of medication – also referred to as a 'non-pharmacological' approach.
Spiritual Care professionals work with patients, families and staff who are experiencing or have experienced delirium. Not only is delirium a medical emergency, it is also a spiritual emergency.
"The hope is by integrating a reflective model into the training already taking place at UHN, we will be able to prevent delirium or shorten its course and intensity," says Moe Anderson, one of the Spiritual Care Professionals who works with delirium. "With patients, families and staff experiencing equally high levels of distress, it is important to address everyone involved in the care of delirium."
While we aim to provide our patients with excellent care, delirium is disconcerting and can lead to post-traumatic stress disorder. The additional time spent in hospital to treat delirium results in significant costs to the health care system – and more importantly – adds more stress to patients and families.
Delirium not only causes patients to experience traumatic events, healthcare professionals also experience high levels of distress and burnout.
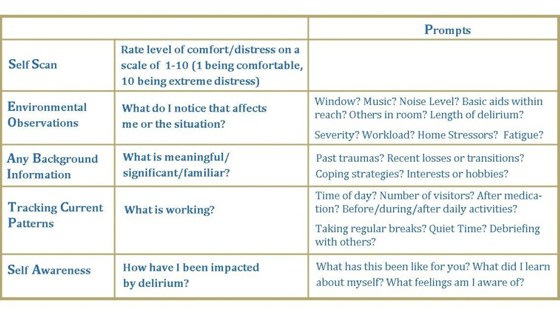
S.E.A.T.S. stands for Self scan, Environmental observations, Any background information, Tracking current patterns and Self awareness. (Photo: UHN)
Delirium: Impact on health professionals
Jeff was a new nurse on the unit. On his first shift, he was faced with a delirious patient. Each time Jeff entered the room, he scanned how the patient was feeling. If he was anxious, he took a couple of deep breaths. The calmer voice and presence helped the patient and family to remain calm. Using S.E.A.T.S., Jeff was able to identify environmental changes he could easily facilitate, even with his busy day.
Spiritual Care hopes to also engage families with the S.E.A.T.S. model so they can help prevent, identify and treat delirium affecting their loved ones. The family of Mr. Smith learned the S.E.A.T.S. model in their pre-surgery clinic.
The day after surgery, the family noticed he was exceptionally quiet and brought this to the attention of his care team. The nurse used the Confusion Assessment Method (CAM), a screening test for delirium, and he was identified as positive. The inter-professional team implemented a care plan to address the delirium, and the family was able to employ all of the strategies they had learned. Within hours, Mr. Smith's condition improved.
Stay tuned for more information on S.E.A.T.S. and how you can learn more about this reflective approach to delirium.
Click here to read more about what you can do to prevent delirium in the hospital.
Editor's note: For privacy purposes, the names of patients and staff members identified in this piece have been changed.
