Michael shares his story of chronic pain, opioid dependence, and overcoming addiction thanks to the Transitional Pain Service at Toronto General Hospital. (Video: UHN)
Fentanyl patches. Hydromorphone. Percocet. Oxycodone. OxyContin.
These are all strong opioids with addictive properties – and each one a medicine that Michael Satok Wolman had been prescribed for various conditions over the course of 20 years.
Due to fibromyalgia, scoliosis, arthritis, Multiple Sclerosis and other diagnoses, Michael, 59, became increasingly tolerant and addicted to the medicines meant to manage his pain.
"I was shackled to the clock," he says.
"I was always waiting for the time to come so I could take my next pill, my next dose."
At the peak, Michael's opioid intake was five times higher than the safe dose – an amount of about 120 mg of hydromorphone.
Then, in 2015, Michael was introduced to the Transitional Pain Service (TPS) at Toronto General Hospital (TGH) and his life took an unexpected turn.
'A life-altering opportunity'
An ulcer that had been growing in Michael's stomach – caused by his intake of ibuprofen in addition to the opioids – burst in early 2015.
Related to this story:
Though he doesn't remember it, he managed to press a button he wears around his neck to call 911. He was rushed to TGH, where his opioid intake was flagged to the TPS during his care.
"At this point, I had recognized I was a prisoner of my own addiction. If someone was going to give me a chance, I was going to take it," he says.
Dr. Hance Clarke, Medical Director of the Pain Research Unit and Director of the TPS in the Anesthesia Department and Pain Management at TGH, and his team offered Michael an opportunity to join their program as a way to gain control of his opioid intake.

For 20 years, Michael’s tolerance of and dependence on opioids continued to increase. (Photo: Michael Satok Wolman)
The Transitional Pain Service aims to treat complex pain patients – often those who have had surgery – by helping with pain control, monitoring and weaning them off excessive amounts of opioid medications for pain. The program also provides support to patients as they transition from their hospital stay back to the community.
Step one of Michael's new pain management strategy was to wean off the opioids that were controlling his life – meaning he would have to purposely propel himself into withdrawal.
Dante's Inferno
After years of building up a tolerance, Michael's opioids were no longer halting the pain. He was simply taking them to ward off the withdrawal and drug sickness. "Opiates crave opiates," he explains.
"I've always been a fan of the Divine Comedy by Dante. Withdrawal is the closest I've been able to come to his descriptions of being in hell.
"Not taking the drugs makes you want to crawl out of your own skin," Michael explains. "You just want to remove yourself from your nervous system."
When opioids are no longer serving their purpose, says Dr. Clarke, they become a problem. For Michael, the fear of withdrawal controlled his life.
A novel approach
Through the TPS, Michael discovered a support system.
Once Michael had put himself through withdrawal from a lack of opioids, with the help of a team of physicians, Dr. Clarke prescribed an alternative medicine to help him manage his pain.
"Within four days I was no longer ill," Michael remembers. "Remarkably, some of the pain in my legs that I'd had for 30 years was gone. I didn't crave the opioids anymore."
The Transitional Pain Team uses many methods to help and teach patients to manage their pain. These include non-opioid medications, psychological techniques such as mindfulness, as well as "exercise prescriptions" and acupuncture by a team of medical pain specialists, pain nurse practitioners, a psychologist and physiotherapists.
"We know that if we're going to take a pain patient and take away their opioids, we need to provide them with alternatives," explains Dr. Clarke. "Otherwise, evidence shows us that without alternatives many patients will turn to street drugs such as heroin."
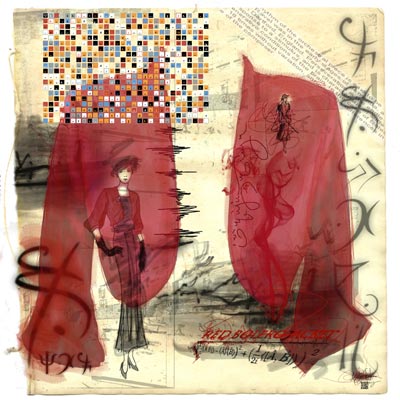
Now that Michael has weaned off opioids, he has more freedom. He is an artist, now focused on digital artwork such as the piece above, entitled ‘Red Bolero Jacket.’ View more of his art
here and
here. (Image: ‘Red Bolero Jacket’ by Michael Satok Wolman)
Alternative pain management techniques give patients a substitute for strong pain medications. For Michael, the support he received through a weekly group meeting led by psychologist Dr. Aliza Weinrib and her team, mindfulness techniques taught by the TPS and other non-opioid medications have made all the difference.
"I'm able to go through life without looking at the clock every three hours," he says.
Michael finds he is more social, feels less isolated and is able to focus on his art.
"I'm able to enjoy my life, which is a good life," he says.
"I feel lucky to have been able to change direction before it was too late. And that's what happened - it's not too late."
