
The Hand Therapy Clinic's (L to R) Teresa Wesolowski, Andrea Rabiewsky and Mary Chang work together putting the finishing touches on a custom splint for the hand transplant patient. (Photo: UHN)
Hand transplantation: the surgical procedure to transplant a hand from one person to another.
That dictionary definition may make it sound like a straightforward, though complex, procedure. But, once the surgery is complete, what does it take for a patient to begin to use their new hand?
Last month, Toronto Western Hospital's (TWH) Hand and Upper Extremity Transplant Program and UHN's Multi-Organ Transplant Program performed
Canada's first hand and forearm transplant.
Having the surgical expertise and resources to successfully transplant a hand is a major medical achievement. However, it isn't as simple as waking up from surgery and having a new hand.
The ultimate success of the transplant lies in the patient's ability to gain feeling and use of their new limb.
Three-person team
Enter a team from TWH's Hand Therapy Clinic.
Physiotherapists Teresa Wesolowski and Mary Chang, along with Occupational Therapist Andrea Rabiewsky, are the Hand Therapy Team working with the hand transplant patient during her recovery.
"Although this is the first patient of its kind that we've had, we're confident our team and clinic has the expertise necessary to deliver the best possible therapy for her," says Teresa. "Treating a transplant patient is somewhat similar to working with patients who have had a complex injury, a nerve injury or a replantation where their hand or fingers are reattached after an accident.
"Between the three of us, we have a lot of experience to draw on and what we learn from working with this patient will benefit future patients of the clinic."
More than 110 transplants have been performed worldwide and each transplant patient is unique. But in general, there are three phases to the recovery process which can take up to two years.
First phase
During the initial phase of recovery, the patient wears a custom-made protective splint over the surgical area to keep the arm in a good position for the bone to heal and avoid any shortening of the muscles and joints. Because the patient can't yet use her arm, stiffness can develop.
The splint prevents tightening of the muscles and joints and also maintains their flexibility until they are strong enough to function again.
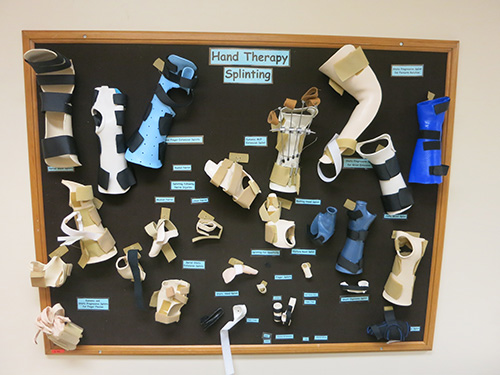
A variety of custom splints made to meet the unique needs of patients in the Hand Clinic adorn the Hand Therapy Splinting board. (Photo: UHN)
The hand therapy team works with the patient to begin range of motion exercises that she does both with them and at home on her own. "The patient is an equal participant and her engagement with these exercises is critical to the success of her recovery," explains Teresa.
Muscle strengthening
Approximately three to four months after the transplant, the muscles in the forearm should start to recover. The patient should notice small muscle movements in her forearm as she regains strength down the length of the arm but she still won't have sensation in her hand.
At this stage, the hand therapy team will work with the patient on strengthening exercises to build up these muscles that haven't been used for a few months as well as how to handle her day to day activities at home.
"This patient was living without a hand for several years and so she has adapted to function without it," says Teresa. "We'll be working with her to incorporate using her new limb into her life."
Movement is vital to function, but feeling is critical
During the transplant procedure, surgeons work delicately to attach the arteries, blood vessels and nerves of the donor limb to the recipient. Although the arteries and blood vessels will immediately begin to circulate blood through the transplanted limb, the nerves take longer to regenerate.
Nerve fibres, like hair, grow about one millimetre per day. Although the muscles will start to work as the nerves grow, gaining feeling in the limb takes longer. It is expected the patient will start to have some feeling in her transplanted hand approximately a couple of years after the surgery.
Sensation to the fingers will be the last part of the recovery.
"Essentially, the patient is growing new nerves," explains Andrea. "Although the nerves have been attached, it's similar to cutting a tree at its root and watching it regrow – the function of the nerve only recovers as it grows."
The patient will work with the hand therapy team to re-educate her sense of touch. She will learn how to touch, how to differentiate between a variety of textures, and identify pressure in the tips of her fingers.
"This last phase is the most critical part of the recovery," says Teresa. "To be able to use your hand, you need to be able to feel it in order to know how much pressure is needed to hold a pen and write, or to pick up a glass."
Proud to be part of a Canadian first
In addition to her long rehabilitation, the patient is also being monitored for any signs of rejection of the limb – something that can occur with any organ transplant.
But despite these challenges, TWH's hand therapy experts are excited and honoured to be part of the care team that is guiding Canada's first transplant patient through this process from beginning to end.
"Because this is our first transplant case, there will be times during the recovery process that decisions will need to be made about what's best for treatment," says Andrea. "But our clinic is unique to UHN in its level of collaboration between experts from surgery to therapy, and that pool of expertise is of great benefit to this patient.
"It's pretty amazing to be part of a team that can provide care to a patient on a level that is life changing."
