Your esophagus is a muscle shaped like a tube. It connects your throat to your stomach. Food travels down this tube and goes into your stomach.
The lining of the esophagus may get damaged by reflux (heartburn), swallowing a poisonous liquid, or cancer. If your esophagus is badly damaged or cancer develops, it must be removed. This is called an esophagectomy.
Pre-Admission Visit
In the weeks before your operation, you will have a pre-admission appointment. This appointment could take 2 to 4 hours, or sometimes longer.
What should I bring to my pre-admission appointment?
- Your health card (OHIP card). If you do not have an OHIP card, please bring another form of government-issued photo ID, such as a driver's license or passport.
- Any other insurance cards. You will need the policy number of your extended health insurance, if you have any.
- Your spouse/partner, a trusted friend or family member (to offer you support and be a second set of ears).
- All the medications you take in their original containers. This includes prescription medications, over-the-counter medicines, vitamins, supplements and herbal or natural products.
- A copy of your power of attorney for personal care and/or advanced directives.
- A list of any questions that you may have about the operation and recovery.
- The name or phone number of your pharmacy, as well as any medical specialists that you have seen in the past 3 years.
- If you have had a cardiac stress test, echocardiogram and/or a pulmonary function test in the past 3 years, it would be helpful to bring a copy of the final report with you to this appointment.
What happens during my pre-admission visit?
- You will have blood tests and routine skin swabs. The swabs are taken from your nose and other areas of your body to check for germs that can cause infections.
- You may also need an
electrocardiogram (ECG) to check your heart and a chest
x-ray to check your lungs.
- You will meet many health care providers during your pre-admission visit. Please feel free to ask them any questions that you may have.
- A pre-admission nurse will review your health history and give you information to prepare you for your operation, including directions for cleaning your skin, eating before your operation, taking your medications and pain management.
- A pharmacist will review your medications.
Depending on your needs, you may also meet:
- An anesthetist who will review your health history, discuss your anesthetic plan and pain relief after your operation.
- A member of the medicine team, if you have other complex health problems.
The night before your surgery
- Do not eat or drink after midnight on the night before your surgery.
- If you smoke, do not do so for 24 hours before your operation.
- Do not drink alcohol for 24 hours before your operation.
- Remove all nail polish and body piercings.
- You must have a shower with soap and water to clean your skin the night before and the morning of your surgery to reduce the chance of infection after your operation.
Stop smoking before your surgery: learn how smoking and tobacco can affect your recovery after surgery, and how
quitting can improve your health.
WHAT SHOULD I DO THE DAY OF MY SURGERY?
Arrive
2 hours before your scheduled operation time.
Surgical Admission Unit (SAU) at
Toronto General Hospital
Peter Munk Building – 2nd Floor
All hospital entrances are open by 6:00 am. However, Elizabeth St. and University Ave. are easiest to access.
You will stay in the
Post Anesthesia Care Unit (PACU) for a few hours. Once you are awake and stable, we will take you up to the
Thoracic Surgery and Respirology Inpatient Unit. You will go to the Step Down Unit (SDU) for close monitoring.
WHAT CAN I EXPECT TO HAVE ON MY BODY?
You will be attached to some or all of these machines and tubes:
| Incisions, tubes or drains | What to expect |
|---|
|
Incisions: If you have an open esophagectomy, you will have 2 or 3 of these incisions (cuts): an incision on your side (thoracotomy), down the middle of your abdomen (laparotomy), and on the side of your neck. If you have a minimally invasive esophagectomy, you will have 5 small incisions on your abdomen. |
|
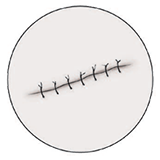
Stitches or staples: Your surgeon usually uses dissolvable stitches to close your incisions. This means they go away on their own. If your stitches or staples need to remain in after you are discharged home, your family doctor can remove them. |
|
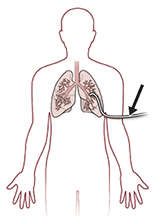
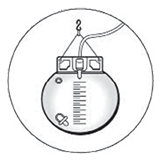
Chest tubes: You will have 1 to 2 chest tubes coming out of the side of your chest that remove air and fluid from the inside of your chest area. The tubes are attached to a machine that helps suck the air and fluid out. |
|
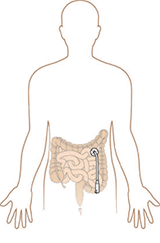
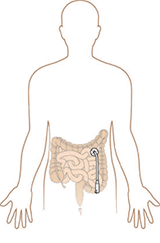
J-tube (Jejunostomy feeding tube): You may have a small tube placed through your abdomen and into your small intestine during your surgery. It is called a J-tube, and it is used to give you liquid food and medicines until you are able to drink and eat well. You will go home with the J-tube still in. |

|
NG tube (nasogastric tube): You will have a small tube called an NG tube coming out of your nose. It was put in during your surgery. It drains fluid, bile (stomach acid) and air from your stomach to help prevent nausea and vomiting. |
|
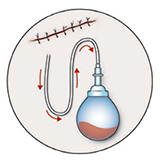
JP drain (Jackson Pratt drain): You will have a small tube called a JP drain that helps drain any extra fluid. It is removed when you no longer need it. |
|
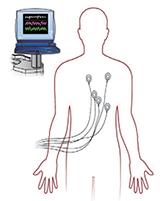
Heart monitor: You will be on a heart monitor while you are in the Step Down Unit. |
|
Urinary catheter: You will have a tube draining your bladder. |

|
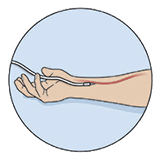
Intravenous (IV): You have an IV so we can give you fluids and medicines. It stays in until you are drinking well. |
|
Arterial line: This tube looks like an IV, and we use it to take blood samples without having to poke you with a needle and also, to closely monitor your blood pressure. |

|
Oxygen: You may need oxygen after your operation. You get the oxygen either by facemask or through your nostrils (nasal prongs). |
HOW CAN I MANAGE MY PAIN?
We will work with you to manage your pain. We can give you pain medicine in different ways:
| Pain relief method | How it works |
|---|
|
Epidural: With an epidural, a doctor puts a small tube in your back. They usually do this right before your surgery. The tube is left in place to give you pain medicine after your surgery. It's attached to a pump, which gives you the medicines. |
|
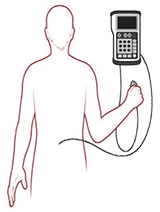
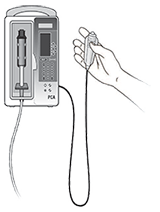
Intravenous (IV) Patient Controlled Analgesic (PCA): A PCA pump is connected to your IV that gives you pain medicine through your IV when you push the button. |
|
Intravenous (IV) medicine: You get your pain medicine through an IV. |
|
J-tube (Jejunostomy feeding tube): You may get your pain medicine through your J-tube. |
|
Medicine by mouth: You may get your pain medicine in tablets that you swallow. This will happen once you are drinking fluids. Let your nurse know when you have pain, so they can give you the pain medicine. |
You will continue to recover when you return home.
| Activity | How to manage at home |
|---|
| - Your appetite and taste should return to normal within a few weeks. Your appetite will improve as you start to feel better and your activities increase.
- Follow the special diet your dietitian gave you. Have smaller meals more often in the day. A large meal will not settle well in your stomach.
- Remember to eat slowly and separate fluids and solids to prevent from filling up too quickly.
- Make sure you drink enough fluids (at least 6 cups a day unless your doctor or dietitian gave you different instructions).
|

| - Diarrhea is common after this surgery. It sometimes helps to separate liquids and solids by 30 minutes, eat a diet with less processed sugars, and avoid dairy products.
- If your pain medicines cause you to become constipated, drink plenty of fluids (unless your doctor or dietitian gave you different instructions).
|
| - Don't cover your incisions unless your clothes are rubbing on them. The J-tube will have a small dry dressing around it.
- Don't put lotions or creams on your incisions until they are completely healed.
- There may be a "bump" along the incisions. It will decrease over 4 to 6 weeks.
|

| - You can shower once you get home. Use a mild soap, and let the water run over your incisions. Pat the incisions dry with a towel. Don’t rub. You can shower with the J-tube in. Dry around the tube and put a dry dressing or bandage on the site after your shower.
|

| - It is normal to feel tired and discouraged for several days or weeks after surgery. Feeling depressed is also common after this surgery. As you recover and improve your strength, this should improve. If you continue to feel depressed as you recover, please see your family doctor. If you are interested in joining our online Esophageal Cancer patient support group, let your nurse coordinator know.
- After this surgery, you should not lie flat. You will need to sleep on a 45-degree angle forever. This can be achieved by a foam-wedge pillow, 6-inch blocks under the head of bed, or an adjustable bed.
- Don't swim, scuba dive or skydive after an esophagectomy.
- Don't jog, do aerobics, or play sports like tennis or racquetball for 4 to 6 weeks.
|

| - You should expect to be off work for at least 4 to 6 weeks. Ask your surgeon when it’s safe for you to return to work.
|

| - No heavy lifting, carrying, pushing or pulling for 4 to 6 weeks. You can lift up to 10 pounds (about 5 kilograms).
|

| - You can start having sex whenever you feel more comfortable. Choose positions that won’t put stress on your incisions.
|
| - Don't drive until you are off all pain medicine. The pain medicine you are taking may make you drowsy. You must be able to fully move your arm and shoulder before you drive. This can take at least 2 to 3 weeks after surgery.
|
| - Please check with your surgeon about travelling. We usually recommend you not travel by air for 2 to 3 weeks.
|
