Recovery After Surgery: Overview
After My Surgery

You have now had your surgery. This part of the guide has more information about your care while in hospital, including:
- What happens after your surgery
- What you need to know about your recovery in hospital
- Taking your medications
- Taking care of yourself
- Managing your pain
- Exercises and activity after your surgery
- Other things you can do
- Caring for your incision
- Taking care of your skin and preventing pressure ulcers
- Rest and sleep
What Happens
What Happens After My Surgery?
After your surgery, we will take you to the
Post-Anesthetic Care Unit (PACU). It is also called the Recovery Room. This room has other patients and may be busy and noisy.
Your nurse checks your pulse and blood pressure often. You may have an oxygen mask that covers your nose and mouth. The nurse calls you by your first name as you wake up and may show you how to do deep breathing and coughing exercises. A member of the operating room team will update your family.
Everyone experiences pain differently after surgery. It is important to tell your nurse if you are having pain.
This page provides more information about how we help you manage your pain and how you can also help yourself.
How long do I stay in PACU?
How long you stay in PACU depends on the care you need, your health and how you recover from the anesthetic. When your condition is stable, we will take you to the nursing unit.
In-hospital Recovery
My Recovery in the Hospital
What happens when I leave PACU and go to the inpatient nursing unit?
While you are on the nursing unit, a team of health care professionals will look after you. You may see different team members depending on your needs.
Your opinion is very important to us. We want you to be as comfortable as possible. Please talk to a member of your health care team about your plan of care each day, or about any questions or concerns you may have.
Taking part in my care: bedside shift report
At shift change, nurses share important information about your care in your room as one nurse is handing over your care to another nurse. This is a time for you to learn more about your plan of care and share important concerns you may have with your nurse. You are encouraged to ask any questions or share your concerns before the shift report begins or ends.
What will I eat and drink?

If needed, you will have an intravenous (IV) line in your hand or arm. This is to give you fluids and medications until you are drinking well.
- You will start drinking liquids as soon as it is safe for you to do so, and if it's right for you.
- Depending on the results of your assessment by your health care team, you may be given solid food to eat.
- Some patients may need a special diet, special meals or a feeding tube after surgery. If you need any of these, your health care team will talk to you about this.
We know that we are not always able to meet the personal food choices of all our patients. We understand that a familiar food brought from home may give you comfort during your hospital stay. Before bringing food from home, talk with your nurse or dietitian first about the kinds of foods that you will be able to have after your surgery.
How will my recovery be monitored?
A member of your health care team will see you every day. If at any time you want to speak with your surgeon or another member of the health care team, please let your nurse know.
The health care team will tell you how you are doing and answer your questions. We check your vital signs (heart rate, blood pressure, temperature, breathing rate and pain score) throughout your hospital stay.
You may have blood tests and diagnostics tests such as
CT scan,
MRI,
x-rays and
ultrasounds after your surgery.
You may need blood tests done every day to monitor a special condition (such as blood sugar levels).
Medications
My Medications
It is important for you to know as much as possible about the medications you will be taking after your surgery, including:
- The name of the medication
- Why you need it
- How much you take
- When you take it
- Any side effects or things you need to know when taking this medication.
When you are ready to leave for your place of residence, we will give you a prescription for any new medications. The nurse or pharmacist will review your medications with you.
Pain
Managing my pain
Review our videos on pain management:
How much pain can I expect after my surgery?
Everyone experiences pain and discomfort differently after surgery. At UHN, we take a holistic (whole body) approach to treating your pain. Our goal is to make sure that you have as little pain as possible after your surgery.
Why is managing my pain important?
It is important to manage your pain because it means you will have less stress on your body. It will:
- help with healing
- decrease complications
- prevent chronic or long-term pain from developing
Managing your pain early helps you to return to your everyday activities much sooner.
How can I tell my health care team about my pain?
At UHN, we use a number scale to measure your pain. We will often ask you to "rate" your pain, when you are moving and when you are resting, using a scale of 0 to 10.
You can use words like
mild, moderate or severe to describe your pain. You can also describe the type of pain you are having. For example, words like sharp, achy and throbbing may help the staff understand and treat your pain better.
Tips for managing my pain
- Keep your pain at a level you can manage (at a rating of 3 or lower on the pain scale). Do not wait until your pain gets worse to ask for pain medication.
- Take your pain medication regularly so you are ready to take part in all activities (such as walking, changing dressing (bandages) or going to the bathroom).
- Depending on the pain medication you are taking, it can take up to 30 minutes to start working. Talk to your health care team about when to take your medication.
Who can help me?
Many members of the health care team can help you manage your pain, including a UHN team of specially trained nurse practitioners and anesthesiologists called the
Acute Pain Service (APS). Also, your Essential Care Partner can help you to be as comfortable as possible after your surgery. Talk about your pain with everyone involved in your care. Your health care team will help you find what works best to manage with your pain.
Exercise
Exercises to Help Me Recover from My Surgery
Review our video on exercises for after your surgery:
You may feel sleepy, and have nausea or be sick to your stomach after your surgery. You may also feel stiff and sore.
These exercises will help you recover from your surgery. Your health care team will let you know if you need to do these exercises once every hour.
Some of these exercises may be uncomfortable for you. Talk to your nurse about managing your pain before starting. This will help you to do these exercises.
1. Breathing with an incentive spirometer 10 times
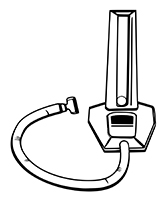
Depending on your surgery and medical history, an incentive spirometer may help you to breathe in as deeply as possible. Breathing deeply helps your lungs work better.
- Breathe in deeply to move the ball to the top.
- Keep the ball at the top for 3 seconds.
- Breathe out.
2. Deep breathing exercises 10 times
These exercises help to clear mucus and keep your lungs well expanded.
- Relax your shoulders. Put your hand on your stomach.
- Breathe in while pushing out your stomach.
- Feel your chest expanding.
- Hold your breath for 3 seconds.
- Breathe out slowly.
3. Splinted cough 3 times

- Position pillow tightly against your incision (if you have had surgery in that area).
- Cough twice in a row and rest in between.
4. Ankle pumping 10 times
It is important to keep the blood moving in your legs. Depending on your surgery, ankle pumping will help prevent blood clots in your veins.
- Lying on your back or sitting in a chair, bend your feet up and down.
5. Leg slides 5-10 times
Depending on your surgery, you may learn how to do leg slides during your Pre-Admission visit.
- Lying on your back, slide your legs up and down by bending your knees.
- Repeat one leg at a time, with your heel slightly off the bed.
When will I be able to do my usual activities again?
You will be able to do more and more activities as time passes, like walking and sitting in a chair for longer periods. Remember that some days you will feel better than others.
You can expect to get up and walk the day of your surgery with help from your nurse or physiotherapist. Each day, we will assess your activity level and help you become more independent.
Handwashing
Handwashing: A Simple Way to Stay Safe
Handwashing is a simple way in which you can help yourself after surgery.
Washing your hands well and often during your stay in hospital can help you stay safe by removing germs from your hands before they can make you sick.
How to wash your hands
- Wet hands
- Apply Soap
- Wash hands for 15 seconds
- Rinse hands
- Dry hands
- Turn taps off with paper towel
How to use hand sanitizer
Rub hand sanitizer between fingers and over both sides of your hands for 15 seconds.
My Incision
How is My Incision Cared for in the Hospital?
After your surgery, you will have an incision (the cut from your surgery) that has been closed with staples or stitches. Your nurse or surgeon may check your incision every day.
- If you have a dressing, your health care team will decide when to remove it.
- You may notice some redness, swelling and oozing of fluid or blood around your incision. Do not be worried. This is normal.
How do I care for my incision after surgery?
Your health care team will show you how to care for your incision before your discharge.
Watch for these symptoms. If you have any of these, call your health care team right away:
- Fever (more than 38 °C or 100 °F)
- New, increasing or worsening redness or swelling at or near your surgery incision
- Pain that suddenly gets worse and is no longer relieved when you take pain medication
- Yellow or green fluid leaking from your incision or more drainage or fluid than before
- Bad smell coming from the incision
Follow these instructions:
- Do not touch your incision.
- Do not remove the scab or paper strips from your incision.
- Do not put lotion, powder or any type of ointment on your incision.
Depending on your surgery, we will decide whether to remove your staples or stitches before you leave the hospital. If you leave with staples still in place, we may give you a staple remover and your family doctor or staff at a walk-in clinic can remove them. If you have questions, ask your nurse or surgeon.
Skin Care
How Can I Take Care of My Skin and Prevent Pressure Ulcers?
Check your skin every day. If you think you are getting skin breakdown, talk to your health care team.
Your skin protects you from infection. You need to protect your skin to protect yourself.
The following sections provide answers on how to take care of your skin.
What is a pressure ulcer?
A pressure ulcer is an area of skin that has been damaged because of pressure from a surface (like a mattress or chair).
You can get a pressure ulcer when this pressure stays for long periods of time over a bony area like your elbow, heel, hips or tailbone.
How do I know I have a pressure ulcer?
Your skin may have different colours at first such as red, purple or blue. The colour does not go away when pressure is removed. This is an important sign from your body that something is causing too much pressure over this area. More skin damage will happen if this pressure continues.
These red, purple or blue areas may become open ulcers, involving your muscles, tendons and bones.
What causes skin breakdown?
There are many reasons that increase the chances of your skin breaking down and leading to pressure ulcers:
- You can't move, you're not moving enough or you're not able to change positions by yourself
- Direct pressure from your bed, chair, wheelchair, or any contact between the equipment and your body
- Friction that happens when you can't lift your body as you change positions in your bed, chair or wheelchair
- Friction that happens when you use your elbows or heels to help yourself move
- Scars from a healed pressure ulcer
- Urine or stool being in contact with your skin often
- Not eating the right kinds of food
- Smoking
- Certain medications
- Certain health conditions
- Aging
What can my Essential Care Partner do to help me?
Have your caregiver look at your skin, paying special attention to areas you can't see or feel well, such as your back, bottom, hips, legs and feet. Watch for any rashes, redness, or open areas.
- Remember your backside!
Moisture from urine, stool and sweat can cause skin breakdown and infections. If your skin is always wet it makes it harder for your skin to protect you. Your skin needs to be cleaned and protected with a barrier cream after each soiling. - Pressure sores begin over bony areas.
Remember to check these areas:
• back • tailbone • bottom • hips • elbows • ankles • heels • shoulder
Tell your health care team about any areas on your skin that are red, purple or blue, painful or open. - Check your feet every day.
Check your feet for red areas, blisters and calluses. Make sure your shoes fit well and are not causing any pressure or friction.
How can I help prevent skin breakdown?
- Change your body position every 2 hours while you are in bed, and every 15 minutes when up in your chair or wheelchair. Your health care team will help you as needed.
- Put a pillow between your legs to prevent your ankles and knees from touching when you are lying sideways in bed. Check with your nurse first to make sure this is right for you.
- Try not to lie directly on your hip bone.
- Make sure your clothes and bed linens are not wrinkled under you.
- Raise your heels off the bed by using 1 or 2 pillows under your lower legs. Or, wear special heel boots.
- Keep the head of your bed as flat as possible so you do not slide down in the bed. Check with your nurse first to make sure this is right for you.
- Have your caregiver use a lift sheet to move you up in bed if you need this type of help.
- Do not use doughnut shaped cushions because they may cause other areas of pressure.
- You may be seen by an Occupational Therapist (OT) who will give you tips on how to best position yourself in your bed or wheelchair. OTs can assess if a pressure reducing cushion or mattress and other assistive devices might help you.
Recovery Tips
What Other Tips Would Help Me?
Skin care tips
- Clean your skin with soap and water, or a special skin cleanser that your health care team recommends. Be sure to pat your skin dry.
- Speak to your health care team about products that keep your skin dry.
- Use a moisturizer on dry skin.
- Put on a barrier cream so that your skin doesn't feel irritated and pressure ulcers don't form.
- Don't rub or massage skin over bony areas. This may cause more skin damage.
Healthy eating tips
- Try to eat and drink regularly if possible.
- You may not be able to eat normally after your surgery. Check with your nurse or doctor to find out what is right for you.
- If you can have regular meals, try to focus on healthy foods. Aim for a variety of foods from each food group (vegetables and fruit, grains, milk and alternatives, meat and alternatives). Refer to Canada's Food Guide for more information.
- Protein is important after surgery to help with healing.
- Meat, chicken, fish, eggs, milk and yogurt are good sources of protein.
- Make sure to drink regularly to stay hydrated. Aim for 6 to 8 cups of fluid through the day, unless your doctor has instructed you differently.
- If you are having trouble eating and drinking or if you have questions about your diet after surgery, ask your nurse or doctor if you can speak to a dietitian.
Activity and exercise tips
Keeping active speeds up your recovery and prevents other health problems.
- Try to get up as soon as possible with help from the staff.
- A Physiotherapist may give you an exercise plan to help you.
- Ask family or a caregiver to help you with exercises.
What about rest and sleep?

It is important for your recovery to get as much sleep and rest as you can after surgery. Have several rest periods during the day.
It is common not to sleep well after surgery. Your sleep will improve as you recover. If you find it hard to sleep at night or you have strange dreams, please let your health care team know, or call your family doctor. Your medications might need to be changed.
