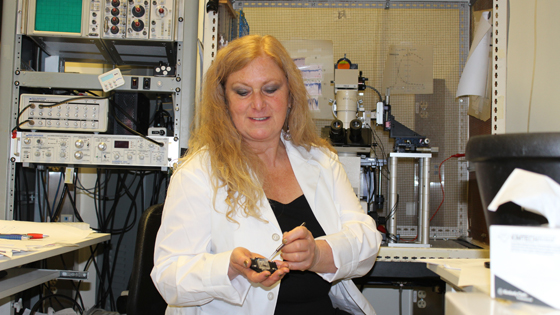
Dr. Lyanne Schlichter prepares a slide of cells. Using the electrophysiology machine behind her, Dr. Schlichter will carefully insert electrodes into the cells, which are 1/10 the width of human hair, in order to record their signals. (Photo: UHN)
June is Stroke Awareness Month. On Wednesday, June 10, join the Krembil Neuroscience Centre's Stroke Program in the atrium of Toronto Western Hospital between 10 and 2 to learn about the warning signs of stroke and how to prevent them.
When it comes to strokes, we know that time is brain. That is, the quicker we receive treatment, the more likely we are to recover.
The majority of research, awareness campaigns and health information focus on those precious minutes between a stroke and receiving medical attention.
But what about the hours, days and weeks
after the initial trauma? What happens to the brain then?
Meet Dr. Lyanne Schlichter, a senior scientist at the Toronto Western Research Institute (TWRI) and professor of Physiology at the University of Toronto, whose life work has focused on the aftermath of stroke and what it tells us about how the brain can heal itself.
Her approach to this research – like much of her scientific career – has been unconventional and even, at times, questioned by her peers. But the novel methods employed by her lab have not only furthered understanding of how the brain is affected by strokes, but also opened up new research avenues for possible treatments.
"I've always been driven by a need to understand how things work, so my research has often taken the less obvious path," Schlichter says. "That's why my research is so focused on trying to understand the disease itself, because once we figure that out, only then can we move on to solve the riddle of how to treat it."
There are many qualities of Schlichter's work that make it unique from other labs studying stroke:
- Her lab is one of only two in Canada that studies both types of stroke: ischemic (when a blood vessel is blocked and the brain is starved of oxygen) and hemorrhagic (when bleeding occurs in the brain), analyzing their similarities and differences in order to find possible treatments.
- In making those comparisons, she is the only researcher using animal models developed to resemble aged humans. Since the chance of stroke doubles every decade after age 55, research models that can replicate these circumstances in the brain will yield better insight into this disease.
- But it is probably her investigation over the past 20 years of the role of inflammation and how it affects the white matter of the brain after a stroke that sets her apart as a pioneer.
Where much stroke research focuses on the brain's grey matter, Schlichter is studying how inflammation after a stroke can damage its white matter – essentially the wire and insulation that the brain's nerve cells use to communicate with each other.
Her lab's work has singled out the brain's own immune cells, called microglia, as a potential culprit in causing this damage. Microglia, like other immune cells, evolved to protect us, but, as Schlichter's research has shown, they can actually be harmful when they sense the brain is injured.
After the first stage of a stroke, the brain enters a secondary phase caused by inflammation. This inflammation, initiated by the microglia, is the immune cells' way of trying to protect the brain from damage. But this innate response is unsophisticated and the cells become overactive in the process, actually causing damage to the white matter that is essential to nerve communication in the central nervous system.
"Decades ago, scientists believed that the only role the brain's immune cells played was as 'garbage men,' cleaning up the debris in a damaged brain," says Dr. Peter Carlen the Scientific Division Head at TWRI who hired Schlichter. "But Dr. Schlichter's work has shown that this inflammation might be contributing to impairment of the brain's white matter, and it will be interesting to see where this discovery takes her."
Today, Schlichter's lab has an international reputation for this work to understand the function of the brain's immune cells. They have identified several molecules that control how the microglia are activated when they sense damage. They now hope to figure out how to better control these cells in order to reduce their harmful properties and help the brain to heal.
"Brain inflammation might not have been a popular choice when I first started studying it 20 years ago, but it's now recognized as a major player in stroke and several other brain diseases," says Schlichter. "In the coming years, I'm determined to figure out how to harness it for brain repair and I'm excited about what this will mean for stroke patients."
