Toronto Centre for Liver Disease
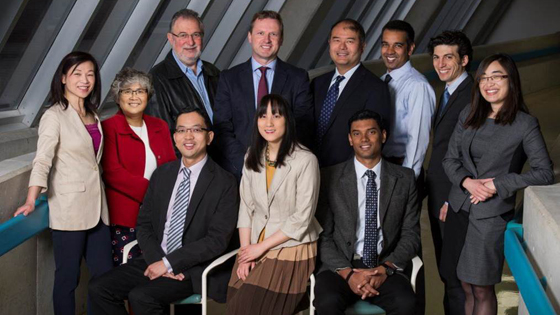
Some of the clinical staff at the Toronto Centre for Liver Disease, which integrates patient care, research and education into one location at Toronto General Hospital. (L to R, back) Nurse Practitioner Colina Yim, Dr. Florence Wong, Dr. Morris Sherman, Director of the Toronto Centre for Liver Disease, Dr. Harry Janssen, Drs. Dave Wong, Hemant Shah, Jordan Feld and Cynthia Tsien. (L to R, front) Drs. Scott Fung, Angela C. Cheung, and Joshua Juan. (Photo: Visual Services UHN)
Liver disease is a growing epidemic and a sense of urgency is needed to diagnose, treat, understand and counter the stigma linked to it, say liver specialists at the Toronto Centre for Liver Disease located at Toronto General Hospital.
Officially opening its doors today, the unique Centre brings together almost 100 staff for both basic and clinical research. It's integrated with a clinic offering patients access to the most advanced treatments, customized care plans, peer-to-peer patient support, outreach into communities, education and expertise in many liver diseases.
"Therapies for liver disease are rapidly evolving," says Dr. Harry Janssen, Director of the Toronto Centre for Liver Disease (TCLD).
"But to take full advantage of this, we need to ensure that individuals with these diseases can access the care they need, including screening programs, diagnosis, state-of-the-art healthcare delivery, research innovation and awareness."
With its focus on rapidly evolving research from the bench to the bedside, the Centre now has the largest liver clinic in North America, more than 100 ongoing clinical research studies, along with genetic studies examining biomarkers for disease outcomes, as well as research on the full spectrum of liver disease – such as viral hepatitis and autoimmune liver disease, fatty liver disease and liver cancer.
"The outstanding expertise in our Centre will allow us to accelerate basic and clinical research discoveries into clinical practice so that patients can benefit at the earliest possible opportunity," explains Dr. Janssen, who is a renowned scientific leader in numerous global studies on anti-viral treatment for viral hepatitis.
"We are the only comprehensive Liver Centre in the Greater Toronto Area, with one of the largest viral hepatitis treatment programs worldwide, as well as many patients from other countries with high rates of viral hepatitis."
Viral hepatitis is more common among some immigrants than among the general population, due to a number of factors, including: unsafe medical practices such as transfusions of contaminated blood, shared needles or other equipment in foreign countries, and barriers to healthcare and testing of immigrants, such as cultural and language obstacles to services and information.
It is estimated that one in five Canadians, or more than five million people, has some form of liver disease. The most common forms of liver disease — viral hepatitis, fatty liver disease and liver cancer — will have huge implications for the burden of care in hospitals and clinics.
As the infected population ages, the incidence of liver disease complications will rise. Due to the slow progression of the illness, infections that occurred decades ago are now beginning to challenge healthcare resources.
Liver cancer is growing rapidly every year, says Dr. Morris Sherman, a Centre physician and leading expert in liver cancer. He points out that the main risk factors for liver cancer are viral hepatitis B and C infections, which are still "invisible" diseases.
Many of those infected with hepatitis are not aware they have it, nor how they acquired the infection.
"It's an epidemic, and it will tax our health care system within the next decade. It's critical that we address this now," he says.
Of
the more than five million Canadians with liver disease, about 500,000 of those
have viral hepatitis. The death rate from chronic viral hepatitis exceeds that of HIV. Less than one in 10 hepatitis B patients and less than 15 per cent of hepatitis C patients have been effectively treated, despite the fact that hepatitis C is now curable, as shown in published research led by Dr. Jordan Feld, physician in the Toronto Centre for Liver Disease.
"Liver disease on the whole is unrecognized in the general population, as it is in health-care professions," says Dr. Feld, who is an international expert in hepatitis C. "There's a stigma linked to this illness that revolves around alcohol and drug use."
"People need to understand there are many causes of liver disease, and that early detection and treatment can prevent the disease from progressing to cancer and death."
Peer support
The Centre's one-of-a-kind, peer-to-peer Chinese support group helps in educating patients about hepatitis B and its treatment options. Hepatitis B is highly prevalent in China, the Philippines and other areas of South East Asia.
Begun by the Centre's Nurse Practitioner Colina Yim, the peer support group usually turns out about 90 patients at each of their events and seminars.
"We answer a lot of questions during these events," Colina says, adding that the group also learns about nutrition and other ways of supporting each other throughout their illness. "We teach them how to have a heathy life, not just a healthy liver."

Larry Wong, 69, is co-founder of the peer support group for patients with hepatitis B at the Toronto Centre for Liver Disease. Shown here golfing in Costa Rica in 2015. (Photo: Larry Wong)
Larry Wong, 69, is a co-founder of the peer support group. Diagnosed as a hepatitis B carrier in 1985 when he tried to donate blood, he did not have any symptoms until about four years later.
He describes feeling exhausted, nauseous and weak. Going to Emergency did not provide any relief, as he was told to go home and rest.
It wasn't until he came to the Liver Clinic that he was put on medication that allows him to lead a normal life, with no symptoms. Larry has been able to take trips to Hong Kong, and to golf resorts in Pebble Beach, Scotland and Costa Rica.
"I'm positive," he says, "I tell the support group if you look after yourself, have good medical care, you'll be fine. I use myself as an example. Here I am. I'm on medication, and I'm enjoying myself. It works!"
